Index
Introduction
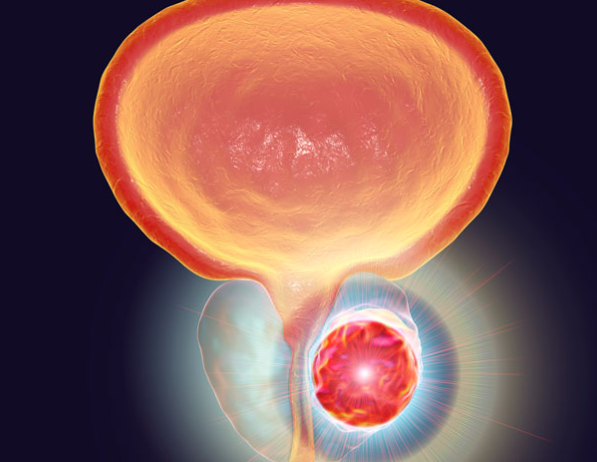
Medicine has crossed previously unimaginable boundaries, driven by technological advancements that transform the lives of patients and doctors. At the heart of this revolution is robotic prostatectomy, an innovative approach to prostate cancer treatment that combines technical precision, reduced invasiveness, and an optimized recovery potential. This procedure not only symbolizes a milestone in modern urology but also reinforces the commitment to excellence in patient care.
The Emergence of Robotic Prostatectomy
Introduced in the early 2000s, robotic prostatectomy represents a significant evolution from traditional surgery. Using the Da Vinci surgical system, this method allows the surgeon to perform the procedure through small incisions, assisted by robotic arms and a high-definition camera. The robot’s precision, capable of more refined movements than the human hand, minimizes the risks of complications, promoting a quicker and less painful recovery for the patient.
The Importance of Robotic Prostatectomy
The significance of robotic prostatectomy goes beyond its technological innovation. It offers patients a less invasive option, with significantly reduced blood loss, lower risk of infection, and shorter hospital stay. Moreover, the prospects for preserving the nerves responsible for erection and urinary control are notably better, addressing two of the main concerns for patients facing prostate cancer treatment.
Advantages Over Traditional Surgery
Compared to traditional surgical techniques, robotic prostatectomy offers clear advantages. The three-dimensional and magnified view of the surgical field provides a detailed perception of anatomy, crucial for surgical precision. This results in a lower rate of intraoperative complications, reduced blood loss, and crucially, better preservation of sexual function and urinary control post-surgery.
The Future is Now: Ongoing Innovation
The evolution of robotic prostatectomy is not stagnant; it continues to expand with the development of new technologies, techniques, and training for surgeons. The future promises even more precision, with the incorporation of artificial intelligence and augmented reality, offering potential to further personalize treatment for each patient, improving surgical outcomes and quality of life after surgery.
What is Robotic Prostatectomy?
Robotic prostatectomy is a watershed in urological surgery, marking a new era in the treatment of prostate cancer. This minimally invasive procedure utilizes advanced robotic technology to remove the prostate affected by cancer, offering unprecedented precision, less pain, and a quicker recovery. Let’s delve deeper into what this means for patients and healthcare professionals.
Technology Ahead of Its Time
- Da Vinci Surgical System
At the heart of robotic prostatectomy is the Da Vinci surgical system, a masterpiece of medical engineering. Comprising a console where the surgeon operates, robotic arms that perform the surgery, and a vision station that provides an enlarged three-dimensional image of the operative field, the Da Vinci enables surgical precision that surpasses the limits of human capability.
- Tools and Capabilities
The instruments of the Da Vinci, functioning as an extension of the surgeon’s hands, are designed to replicate hand movements with even greater range of motion. This means the surgeon can perform delicate sutures and precise cuts that would be extremely difficult, if not impossible, with conventional techniques.
The Origins of the Procedure
- Steps of Robotic Prostatectomy
Robotic prostatectomy begins with small incisions in the patient’s abdomen, through which the robotic arms and camera are inserted. The surgeon, seated at a console within the same operating environment, controls the robotic arms while viewing a high-definition 3D image of the surgical field. The precision of the system allows for the removal of the prostate and affected adjacent tissues, minimizing damage to healthy tissues and surrounding nerves.
- Undeniable Benefits
Robotic surgery offers significant advantages over traditional techniques. Besides enhanced precision and control, patients experience less post-operative pain, reduced risk of infection and bleeding, and a shorter recovery time. This not only improves the surgical experience but also speeds up the return to normal daily activities.
Innovation in Action
- Training and Education
Implementing robotic prostatectomy is not just about technology; it also involves extensive training for surgeons. Certification programs and realistic simulations are crucial for preparing healthcare professionals to effectively operate the Da Vinci system, ensuring that the technology is utilized to its fullest potential for the benefit of patients.
- Challenges and Solutions
Although robotic prostatectomy represents a significant advancement, it also brings challenges, such as the cost of technology and the learning curve for surgeons. However, the tangible benefits to patients and the growing accessibility of technology are helping to overcome these hurdles, making robotic surgery a viable option for an increasing number of cases.
The Future of Urological Surgery
Robotic prostatectomy is just the beginning. With continuous advancements in robotics, artificial intelligence, and data analytics, the field of urological surgery is set for even greater transformation. These technologies promise not only to improve surgical outcomes but also to personalize treatments to meet the individual needs of patients, marking the beginning of a new era in personalized medicine.
Benefits of Robotic Prostatectomy
Robotic prostatectomy represents a milestone in the evolution of surgical treatment for prostate cancer. Its benefits extend beyond the mere effective removal of cancerous tissue, offering significant advantages in terms of patient recovery, reduced risks, and surgical outcomes. Let’s explore these transformative benefits in detail.
Shorter Hospital Stay
- Accelerated Recovery
One of the most immediately noticeable benefits of robotic prostatectomy is the shorter required hospital stay. Thanks to smaller incisions, which result in less pain and risk of complications, patients often experience a faster recovery, allowing them to return to the comfort of their homes and the normality of their lives much sooner than would be possible with conventional surgery.
Reduced Risk of Infection
- Controlled Environment
The precision of robotic prostatectomy minimizes trauma to surrounding tissues, which in turn reduces exposure to potential sources of infection. Additionally, the controlled environment and minimally invasive technique contribute to a lower rate of post-operative infections, a crucial benefit for patient recovery.
Faster Recovery
- Return to Normal Activities
The minimally invasive approach of robotic prostatectomy not only reduces hospital stay time but also positively impacts the overall recovery period. Patients report less post-operative pain and discomfort, which facilitates a quicker return to daily and professional activities. This benefit is essential for the patient’s quality of life during the recovery period.
Enhanced Surgical Precision
- Superior Outcomes
Robotic technology provides unmatched precision, allowing for more precise cuts and preservation of adjacent healthy tissues. This precision is crucial for avoiding damage to nerves responsible for urinary and sexual function, a particularly important aspect for patients undergoing prostate cancer treatment. The ability to perform surgery with such a level of detail results in better functional outcomes and a lower incidence of post-operative complications.
Transforming Prostate Cancer Treatment
Robotic prostatectomy is not just a procedure; it’s a revolution in prostate cancer treatment. The advantages it offers in terms of shorter hospital stays, accelerated recovery, reduced risks, and surgical precision transform the surgical experience for patients worldwide. As the technology continues to evolve, we can expect even further improvements in outcomes and post-operative quality of life for patients.
With the ongoing advancement of robotic technology, medicine is on the brink of new discoveries that promise to further elevate the standard of care. The integration of artificial intelligence for surgical data analysis and precision enhancement, along with the adoption of innovative training techniques for surgeons, are just a few of the future developments that can expand the boundaries of what is possible in prostate cancer surgery.
The Process of Surgery
The journey of robotic prostatectomy is a path of precision, care, and innovation, aimed at delivering the best possible results with minimal discomfort for the patient. This surgical journey comprises several crucial stages, each playing a vital role in the preparation, execution, and recovery of the procedure.
Preparation for Surgery
- Consultation and Evaluation
Before the surgery, patients undergo a detailed consultation and medical evaluation to ensure they are ideal candidates for robotic prostatectomy. This process may include blood tests, biopsies, magnetic resonance imaging (MRI), or computed tomography (CT) scans to assess the extent of prostate cancer.
- Pre-operative Instructions
After confirming eligibility for the surgery, patients receive specific pre-operative instructions. This may involve adjustments in medication, dietary recommendations, and guidelines on physical preparation for the surgery. The goal is to minimize any risk and prepare the body for the procedure and subsequent recovery.
The Day of Surgery
- Arrival and Preparation
On the day of the surgery, patients arrive at the hospital or surgical center and are prepared for the procedure. This includes the administration of general anesthesia, after which the patient is taken to the operating room where the surgery will be performed.
- Execution of the Procedure
Under the command of the Da Vinci surgical system, the surgeon performs the prostatectomy with the assistance of robotic arms. Through small incisions, the surgeon manipulates the robotic instruments to remove the prostate and any surrounding tissues affected by cancer.
Immediate Recovery
- Post-operative Care
Immediately after the surgery, patients are taken to a recovery unit, where the medical team monitors their vital signs and pain level. The immediate recovery from anesthesia is closely followed, and measures are taken to prevent complications such as deep vein thrombosis (DVT) and infections.
The Recovery Phase
- Recovery in the Hospital
The hospital stay following robotic prostatectomy is remarkably short, thanks to the minimally invasive nature of the procedure. During this time, patients receive care to manage pain, support to regain mobility, and instructions for caring for the incisions.
- Recovery at Home
Once home, patients follow a detailed recovery plan, which includes incision care, pain management, and activities to promote healing. Follow-up appointments are scheduled to monitor progress and adjust any aspect of the recovery plan as necessary.
Return to Normal Activities
- Rehabilitation and Follow-up
Rehabilitation plays a crucial role in recovery, focusing on restoring urinary and sexual function. Physiotherapy programs and specific exercises may be recommended to expedite recovery and improve long-term outcomes.
- Ongoing Evaluation
Follow-up after robotic prostatectomy includes regular assessments to monitor the patient’s health and the effectiveness of the procedure. PSA (prostate-specific antigen) tests are periodically conducted to detect any signs of cancer recurrence.
Throughout the entire process, from preparation to recovery, the patient’s experience is a priority. The minimally invasive approach of robotic prostatectomy, along with continuous support from the medical team, aims to ensure that patients feel cared for, comfortable, and informed at every step of the way.
The journey of robotic prostatectomy reflects a commitment to excellence in medical care, combining cutting-edge technology with a patient-centered approach to treating prostate cancer. This process not only seeks to cure but also to improve the quality of life for patients, offering a path to quick recovery and optimized long-term results.
Recovery and Post-Operative Care
After a robotic prostatectomy, the patient’s recovery journey is as important as the surgery itself. Adhering to a carefully crafted post-operative care plan can mean the difference between a smooth recovery and facing unnecessary challenges. Here are some essential guidelines for navigating this critical period.
Pain Management
- Effective Strategies
After surgery, it is normal to experience some degree of discomfort or pain. The medical team will provide guidance on managing pain, which may include prescribed medications, relaxation techniques, and comfort measures such as using cushions for support. Closely following these guidelines will help keep discomfort to a minimum and facilitate a faster recovery.
Physical Activity and Rest
The balance between physical activity and rest is crucial for a successful recovery. In the first weeks after surgery, light activities such as short walks indoors are encouraged to promote circulation and prevent the formation of blood clots. However, it is important to avoid strenuous efforts, weight lifting, or activities that strain the abdominal area to prevent complications.
Incision Care
Proper incision hygiene is vital to prevent infections. The medical team will provide specific instructions on how to care for the incisions, including how to clean them and how often. It is essential to keep the area clean and dry and to report any signs of infection, such as redness, swelling, or drainage, to the medical team immediately.
Nutrition and Hydration
- Healthy Eating
A nutritious, fiber-rich diet can help prevent constipation issues, common after surgery, especially when pain medications are used. Including fruits, vegetables, whole grains, and lean proteins in the diet, along with staying well-hydrated, are important steps to support the healing process and overall recovery.
Monitoring Urinary Function
Temporary changes in urinary function are common after robotic prostatectomy. There may be a need to use a urinary catheter temporarily. The medical team will guide how to manage this and provide Kegel exercises or other techniques to strengthen the pelvic muscles and improve urinary control over time.
Return to Daily Activities
- Gradual and Cautious
The return to normal activities should be gradual and under medical guidance. The ability to resume work or other daily activities varies from patient to patient, depending on the nature of the work and individual recovery. Open discussions with the medical team about when to resume specific activities will help ensure that this return is done safely and at the right time.
- Follow-up Appointments
Follow-up appointments are essential to monitor recovery, assess urinary and sexual function, and ensure that there are no signs of cancer recurrence. These appointments are also an opportunity to discuss any concerns or issues that may arise during the recovery.
The recovery from robotic prostatectomy does not end with the healing of the incisions or the return to everyday activities. Maintaining a routine of regular check-ups, adopting a healthy lifestyle, and communicating openly with the medical team are fundamental steps to ensure the best long-term quality of life.
The post-prostatectomy robotic recovery journey is a unique experience for each patient, involving challenges and achievements. By following these guidelines and maintaining clear communication with healthcare professionals, patients can navigate this period with confidence, towards a complete recovery and a healthy future.
Results and Expectations
After deciding on robotic prostatectomy, understanding the expected outcomes, success rates of the procedure, and potential risks or complications is crucial for patients. This section aims to clarify these aspects, providing a solid foundation for post-surgical expectations.
Typical Outcomes of Robotic Prostatectomy
- Effective Cancer Removal
One of the primary goals of robotic prostatectomy is the complete removal of prostate cancer. Advances in robotic technology offer unprecedented precision, increasing the likelihood of removing all cancerous tissue while preserving the surrounding healthy tissue. This translates into high success rates in eliminating cancer for patients in the early stages of the disease.
- Recovery of Urinary and Sexual Function
Although there may be concerns about urinary and sexual function after surgery, many patients experience significant recovery of these functions over time. The use of nerve-sparing techniques can improve the chances of maintaining erectile function and urinary control, with most patients observing improvements within a year after surgery.
Success Rates
- Survival and Quality of Life
The success rates of robotic prostatectomy are highly encouraging, with many studies reporting excellent long-term cancer-free survival rates. Additionally, the minimally invasive approach contributes to an improved quality of life during the recovery period and beyond, compared to more invasive methods.
Side Effects and Complications
- Urinary Incontinence and Erectile Dysfunction
Two of the most commonly discussed side effects after robotic prostatectomy are urinary incontinence and erectile dysfunction. While most patients experience significant improvement in these conditions over time, it is important to have realistic expectations and discuss management and treatment strategies with your medical team.
- Other Potential Complications
Although less common, other complications may include issues with incision healing, infections, and risks associated with anesthesia. Following post-operative care guidelines and maintaining open communication with the healthcare team are crucial for minimizing these risks.
Navigating Recovery
- Post-Operative Monitoring
After surgery, ongoing monitoring is essential to assess the effectiveness of the treatment and identify any early signs of cancer recurrence. Regular PSA tests are an important part of this follow-up, offering valuable information about the cancer status.
- Support and Rehabilitation
To address side effects such as incontinence and erectile dysfunction, specific rehabilitation programs, including pelvic physiotherapy and sexual counseling, may be recommended. These programs are designed to help patients recover function and improve quality of life.
Setting Realistic Expectations
It is crucial for patients to have realistic expectations about the outcomes of robotic prostatectomy. While the surgery offers a high success rate in removing cancer, the recovery journey is unique for each individual. Frank and detailed discussions with the healthcare team about what to expect can help prepare patients for the recovery process and adjust their expectations accordingly.
Conclusion
Robotic prostatectomy is an effective treatment option for prostate cancer, offering promising results and a relatively quick recovery with less discomfort. Understanding the typical outcomes, success rates, and potential side effects or complications is essential for patients preparing for the procedure. With adequate support, post-operative monitoring, and a commitment to rehabilitation, patients can successfully navigate their recovery, aiming for a long and healthy life after prostate cancer.